U.S. health officials struggled to get public to cooperate with coronavirus contact tracing, new CDC study says
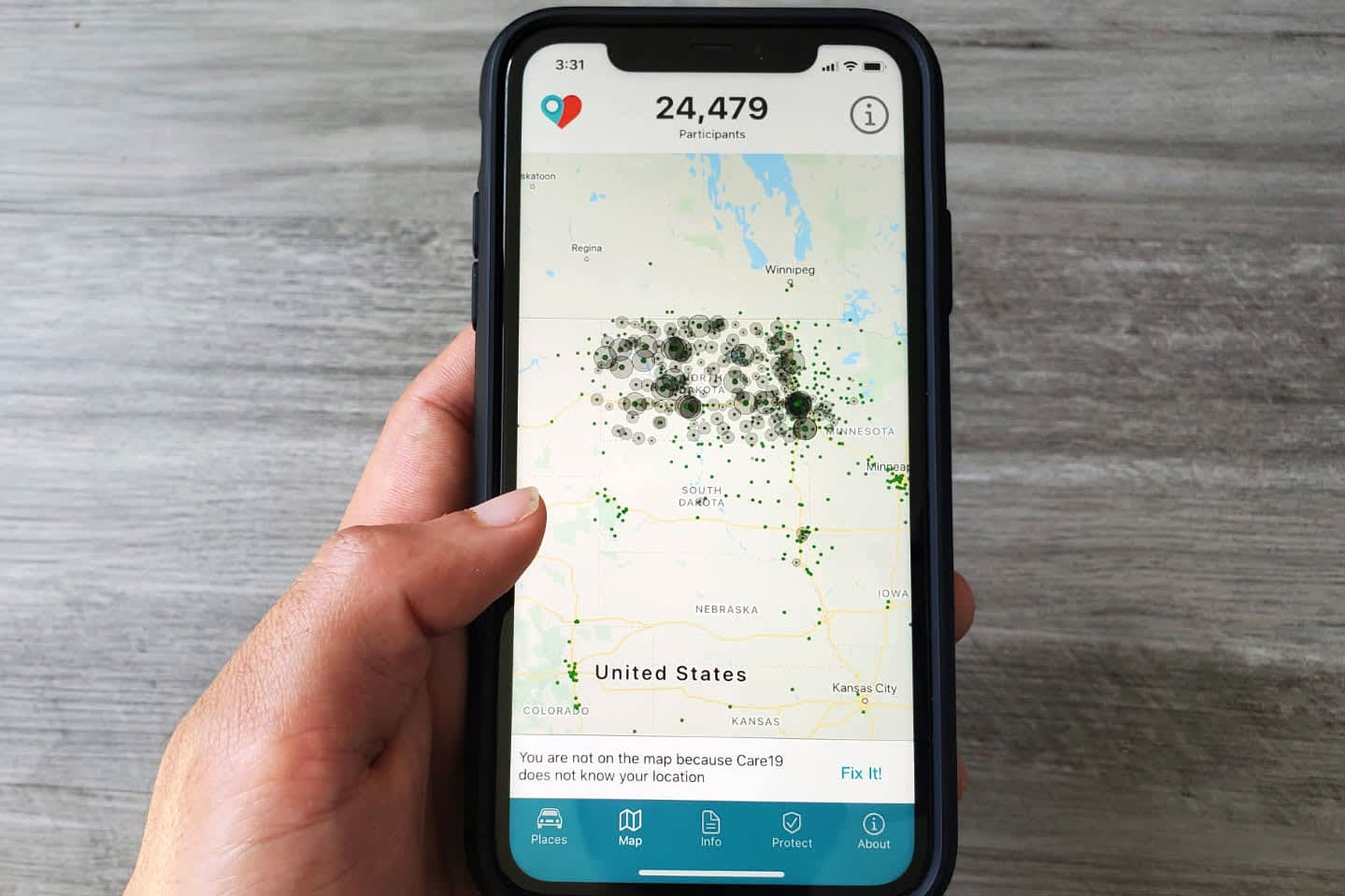
The Care19 mobile app, which the governors of North Dakota and South Dakota have asked residents to download to assist in contact tracing during the global outbreak of the coronavirus disease (COVID-19), is seen on a phone, April 24, 2020.
Dave Paresh | Reuters
Despite “aggressive” efforts to ramp up contact tracing, health departments are struggling to get people to participate in outbreak investigations, according to a study published Tuesday by the Centers for Disease Control and Prevention that focuses on two counties in North Carolina.
Contact tracing is the process through which trained personnel contact those who have tested positive for the virus and identify who they might have exposed to the virus. Health officials then provide potentially infected people with information and encourage them to isolate in order to stop the spread of the virus.
Along with social distancing and mask wearing, contact tracing is one of the only proven strategies in containing the coronavirus and cutting off chains of transmission before they balloon into outbreaks. However, tracing specialists have warned that contact tracing has never been demanded on the scale called for by the pandemic. To ramp up coronavirus contact tracing efforts, specialists have said it would take significant investment from the federal government as well as an overhaul of local health departments.
Researchers of the new study examined tracing efforts in Mecklenburg and Randolph counties in North Carolina between June 1 and July 12. As cases rose in both counties, up to half of people reported not coming into contact with anyone. Of the contacts that were provided to local health authorities, investigators were not able to contact between a quarter and nearly half of them.
“Despite aggressive efforts by health department staff members to perform case investigations and contact tracing, many persons with COVID-19 did not report contacts, and many contacts were not reached,” the authors of the study said. “The relatively low participation and cooperation with contact tracing suggests a lack of community support and engagement with contact tracing. This, coupled with delays in testing results are contributing to ongoing transmission.”
In Mecklenburg County, one of the most populous counties in North Carolina and home to Charlotte, contact tracers investigated 5,514 people with confirmed Covid-19 infections. Among them, 48% reported not coming into close contact with anyone. Among contacts that were provided to contact tracers, 25% of people did not return phone calls from tracers, the researchers said.
In more rural Randolph County, the local health department investigated 584 people with confirmed infections. Of them, the researchers said, 35% of people reported no close contacts and of the contacts that were provided, tracers were only able to successfully contact 52% of potentially exposed people.
The researchers noted that the data found in their study is consistent with that found in other states across the country. They added that the proportion of people who could not be successfully contacted for tracing is higher than that of contact tracing efforts for other infectious diseases in the U.S. before the pandemic.
“There are a few probable reasons for this. First, limiting contact tracing to a telephone conversation might have inhibited the ability of public health workers to establish a rapport and elicit contacts,” they wrote. “Second, persons with COVID-19 might have sought to avoid subjecting their contacts to quarantine control measures, including potential loss of work and related economic consequences.”
Some people might have been reluctant to answer phone calls from unidentified sources, the researchers said. They added that because their study took place while cases were rising in the area, the increase in the burden of outbreak on contact tracers might have also played a role in hampering their performance. But they added that “failure to comply with public health recommendations might reflect the various, and at times conflicting, messages about the importance of COVID-19 mitigations strategies.”
“This assessment revealed that, although these two county health departments investigated the majority of index cases, a high proportion of persons with COVID-19 did not report contacts, many contacts were not reached, and the time needed to notify contacts likely reduced the impact of contact tracing as a mitigation strategy,” the authors concluded. “These findings indicate that improved timeliness of contact tracing, community engagement, and increased use of community-wide mitigation are needed to interrupt SARS-CoV-2 transmission.”




